Imaging the Nigrosome 1 in the substantia nigra using susceptibility weighted imaging and quantitative susceptibility mapping: An application to Parkinson’s disease
By: Karen Holzberger, President & CEO of SpinTech MRI
Author(s): Zenghui Chenga,1 , Naying Hea,1 , Pei Huangb,1 , Yan Lia , Rongbiao Tanga , Sean K. Sethic,d , Kiarash Ghassaband,e , Kiran Kumar Yerramsettyf , Vinay Kumar Palutlaf , Shengdi Chenb,⁎ , Fuhua Yana,⁎ , E. Mark Haackea,b,c,d,e
Journal: NeuroImage: Clinical
Published: 2020
Read Full Paper: https://www.sciencedirect.com/science/article/pii/S2213158219304504?via%3Dihub
Abstract
Parkinson’s disease (PD) is a clinically heterogeneous chronic progressive neuro-degenerative disease with loss of dopaminergic neurons in the nigrosome 1 (N1) territory of the substantia nigra pars compacta (SNpc). To date, there has been a major effort to identify changes in the N1 territory by monitoring increases of iron in the SNpc. However, there is no standard protocol being used to visualize or characterize the N1 territory.
Therefore, the purpose of this study was to create a robust high quality, rapid imaging protocol, determine a slice by slice characterization of the appearance of N1 (the “N1 sign”) and evaluate the loss of the N1 sign in order to differentiate healthy controls (HCs) from patients with PD.
Method
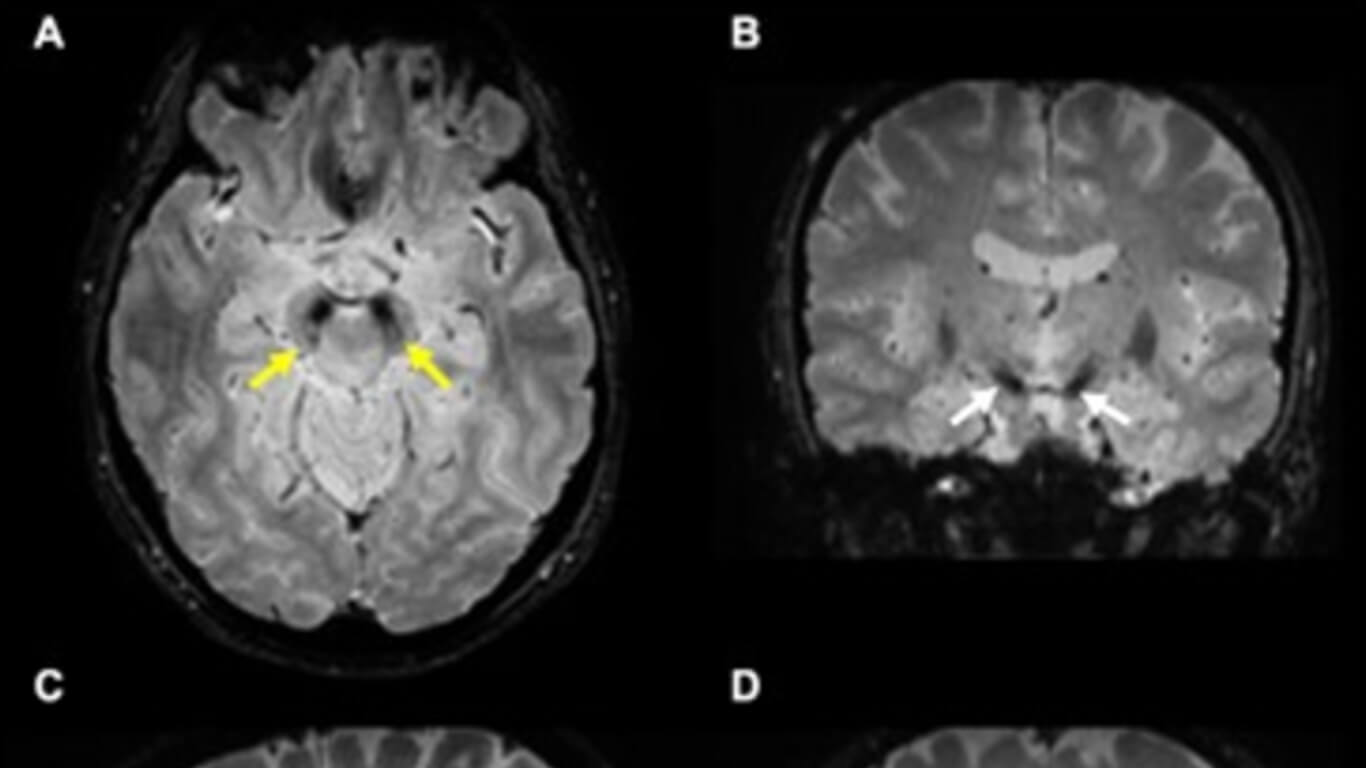
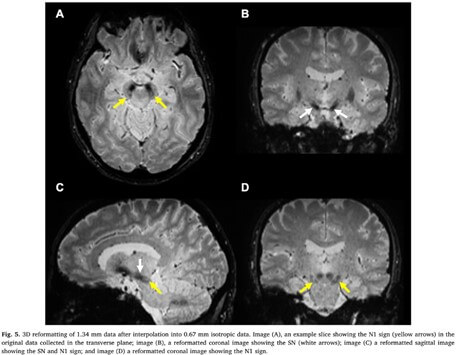
Firstly, one group of 10 HCs was used to determine the choice of imaging parameters. Secondly, another group of 80 HCs was used to characterize the appearance of the N1 sign and train the raters. In this step, the magnitude, susceptibility weighted images (SWI), quantitative susceptibility maps (QSM) and true SWI (tSWI) images were all reviewed using data from a 3D gradient recalled echo sequence. A resolution of 0.67 mm × 0.67 mm × 1.34 mm was chosen based on the ability to cover all the basal ganglia, midbrain and dentate nucleus with good signal-to-noise with echo times of 11 ms and 20 ms. Thirdly, 80 Parkinsonism and related disorders patients [idiopathic Parkinson’s disease (IPD): 57; atypical parkinsonian syndromes (APs): 14; essential tremor (ET): 9] and one additional group of 80 age-matched HCs were blindly analyzed for the presence or absence of the N1 sign for a differential diagnosis.
Results
From the first group of 80 HCs, all of the 76 (100%) cases (4 were excluded due to motion artifacts) showed the N1 sign in one form or another after reviewing the first 5 caudal slices of the SN. For the second group of 80 HCs, 78 (97.5%) showed the N1 sign in at least 2 slices. Of the 80 Parkinsonism and related disorders patients, 32 (56.1%, 32/57) IPD and 6 (42.9%, 6/14) APs showed a bilateral loss of the N1 sign, 12 (21.1%, 12/57) IPD and 6 (42.9%, 6/14) APs showed the N1 sign unilaterally and 13 (22.8%, 13/57) IPD and 2 (14.2%, 2/14) APs showed the N1 sign bilaterally. Also, all 9 (100%, 9/9) ET patients showed the N1 sign bilaterally. The mean total structure and mean high susceptibility region for the SN for both IPD and APs patients with bilateral loss of N1 were higher than those of the HCs (p < 0.002).
Conclusions
The N1 sign can be consistently visualized using tSWI with a resolution of at least 0.67 mm × 0.67 mm × 1.34 mm and can be seen in 95% of HCs.

